Abstract
Focal adhesion kinase (FAK), activated by integrins and cytokines, promotes cell growth, migration and metastasis. We previously reported that a selective FAK inhibitor, VS-4718, inhibited cell growth and induced cell death in leukemia cell lines in vitro, effectively reduced leukemia burden in peripheral blood and tissues including bone marrow, spleen, liver and lung, and significantly prolonged survival time in a human xenograft murine model (Carter BZ et al., MCT, 2017), 16(6):1133).
Although BCL-2 inhibition by the BCL-2 inhibitor ABT-199 (Venetoclax) has demonstrated antileukemia activities, an acquired drug resistance frequently ensues. When combined with ABT-199, VS-4718 significantly potentiated ABT-199-induced apoptosis in AML cell lines and primary AML cells. VS-4718 treatment of Molm14 AML cells decreased levels of p-STAT5, MCL-1, and BCL-XL (Wang et al., ASH 2016) that play important roles in the acquired resistance to ABT-199.
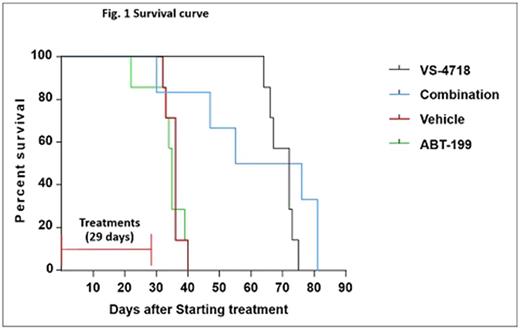
To further examine the effect of VS-4718 as a single agent and in combination with ABT-199 on primary AML cells in vivo, we generated patient-derived xenografts (PDX) from AML patient bone marrow cells expanded in NSGS (NOD-SCID IL2Rgnull-3/GM/SF, NSG-SGM3) mice. The xenograft used AML cells from a patient who had failed multiple chemotherapies and had NPM1, FLT3-ITD, TET2, DNMT3A, and WT1 gene mutations and a complex karyotype. The combination of VS-4718 and ABT-199 synergistically killed the PDX cells in vitro even under MSC co-culture conditions. Once PDX cells were engrafted into NSGS mice, animals were randomized into 4 groups (N=10/group) and treated with vehicle, VS-4718 (75 mg/kg, twice daily), ABT-199 (100 mg/kg, once per day), or the combination via oral gavage for 29 days. We observed that ABT-199 had a stronger anti-leukemic effect on peripheral blood than on tissue-resident cells, while VS-4718 was more effective in tissues. At the end of the treatments, VS-4718 significantly reduced circulating human CD45+ cells (P=0.0003), and ABT-199 alone (P=5.90E-07) and the ABT-199/VS-4718 combination (P=5.38E-07) were ever more effective. VS-4718 alone or in combination with ABT-199 reduced leukemia burden in spleen and liver and effectively reduced splenomegaly, while ABT-199 alone did not. VS-4718-treated mice survived significantly longer than the untreated controls (median survival 72 vs. 36 days, P=0.0002), while ABT-199 did not prolong survival (median survival 35 days). Also, the combination of VS-4718 with ABT-199 significantly prolonged survival (median survival 65.5 days, P=0.011 vs. control and P=0.0072 vs. ABT-199). No statistical difference in survival was found between VS-4718 and the combination treatment groups (P=0.33) (Fig. 1). All the mice had large spleen at death except the combination group: the 1st dead mouse had small and the 2nd to 4th ones had slightly enlarged spleen and only the last two had large spleen as others suggesting that additional reasons such as toxicity at the dose used may have contributed to the death of the 1st 4 mice in the combination group, hence shortened the median survival in this group.
We determined expression of FAK and BCL-2 family proteins in cells from mouse spleens at the end of treatment and found that the combination of VS-4718 and ABT-199 decreased protein levels of FAK. Consistent with our in vitro results, the increased level of MCL-1 by ABT-199 was antagonized by the combination with VS-4718 in vivo suggesting the combination potentially be more effective.
Conclusions: These results suggest a potential clinical benefit of combining a FAK inhibitor with Venetoclax for patients with AML.
Pachter: Verastem, Inc.: Employment. Weaver: Verastem, Inc.: Employment. Carter: Daiichi Sankyo: Research Funding; novartis: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal